Shoulder (glenohumeral) arthritis
Shoulder Arthritis and shoulder replacement
NORMAL SHOULDER ANATOMY
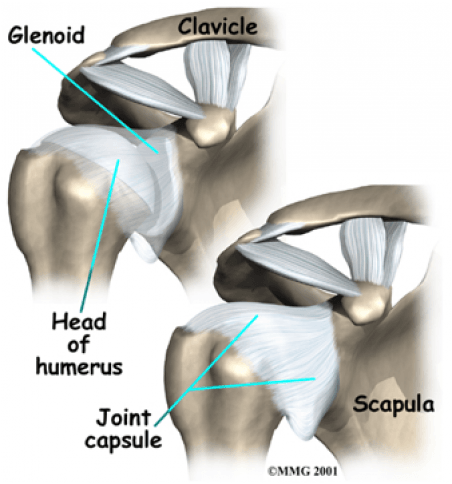
The shoulder is made up of three bones: the scapula (shoulder blade), the humerus (upper arm bone), and the clavicle (collarbone). The rotator cuff connects the humerus to the scapula, and its function is to keep the humeral head (ball) on the glenoid (the socket), and it is important to help raise and rotate the arm.
A part of the scapula, called the glenoid, makes up the socket of the shoulder. The glenoid is shallow and flat. The humeral head of the shoulder is the ball portion of the joint. Articular cartilage is the smooth, white material that covers the ends of bones in most joints. Articular cartilage provides a slick, rubbery surface that allows the bones to glide over each other as they move. Cartilage also functions as sort of a shock absorber.
SHOULDER (GLENOHUMERAL) ARTHRITIS
Arthritis of the shoulder, or glenohumeral arthritis, affects the glenohumeral cartilage in the shoulder. When cartilage is damaged, there can be pain, decreased motion, abnormal bone formation (bone spurs), and weakness.


Causes of shoulder arthritis
Destruction of the glenohumeral cartilage occurs as a result from:
- Osteoarthritis
- Rheumatoid arthritis
- Postraumatic arthritis
- Rotator cuff tears
- A history of shoulder fractures or dislocations
- Repetitive overhead lifting, such as that done by weightlifters or construction workers who reach overhead, can increase the incidence of the disease.
Signs and symptoms of arthritis of the shoulder
One of the first signs that a person may have glenohumeral arthritis is pain and tenderness in the shoulder area and upper arm. Patients often describe a knife-like sharp pain radiating from the back of the shoulder to the front. Sometimes patients will report pain in the forearm. Loss of motion is common, especially external rotation. Compression of the joint, which may occur when picking up an object away from the body, will cause pain. Patients with arthritis of the shoulder will have trouble doing everyday activities, like reaching overhead, washing their back, or sleeping on their affected side.
Shoulder arthritis diagnosis
Most of the information to diagnose arthritis comes from the patient’s symptoms. On physical exam, the physician will often notice decreased motion, especially external rotation. Crepitus, or the sensation of grating, can be felt or heard with motion. Patients will often describe a knife-like pain when they attempt to lift objects away from their body. Occasionally, an injection directly into the glenohumeral joint (not into the subacromial space, which is done for rotator cuff problems) is given. This should relieve symptoms at least temporarily if arthritis is present.
X-rays are obtained to evaluate for joint space narrowing and spur formation. It is imperative that an axillary x-ray is obtained to determine if there is bone loss in the posterior glenoid. If there is too much bone loss some surgical options are lost because the glenoid (the cup) will not support a prosthesis. MRI and CT scans are generally required to evaluate arthritis. An MRI is obtained if there is a question to the integrity of the rotator cuff and a CT scan may be obtained if the amount of bone loss must be further evaluated.


Shoulder arthritis treatment
Treatment is initially conservative.
- Anti-inflammatory medication (Advil, ibuprofen, naproxen), ice, and avoidance of aggravating activities are first attempted.
- A corticosteroid injection into the glenohumeral joint may be tried. Most studies have shown approximately 6 to 8 weeks of relief from these injection, and this is not a permanent solution.
- Physical therapy: This may be considered, but often increased motion will aggravate the pain associated with arthritis.
Shoulder replacement – if all conservative options have been exhausted, the next treatment is usually a total shoulder replacement. The ball portion of the joint is replaced with an alloy metal ball attached to a metal stem to hold the ball in position. The glenoid, or cup, is replaced with a polyethylene (plastic) tray. At times there are reasons that only the ball portion of the shoulder can be replaced due to patient or surgical considerations.


TOTAL SHOULDER REPLACEMENT OUTCOME
How common is the procedure?
While not as common as knee and hip replacements, total shoulder replacement is a very well established procedure which has been performed for more than 3 decades. There is significant increase in number of shoulder replacements being done in the US, and annually there is about 50,000 such procedures performed.
What is the success rate?
Shoulder replacement patients are the happiest patients in a shoulder practice because they often have had long standing shoulder pain, and shoulder replacement is very reliable in providing pain relief and functional improvement. When 200 patients who had shoulder replacements are asked at one year mark after surgery, 98% of the patients are satisfied or very satisfied.
How long do the shoulder replacements last?
In long term follow up studies of total shoulder replacements, at 10 years after surgery, approximately 93% of the people are doing well with the original prosthesis, and at 20 years, 84% of the patients still have their original replacement. These data are based on older generations of implants. In the last decade, there is improvement in surgical technique, better understanding of shoulder biomechanics, and superior implant technology. So survivorship of the shoulder replacements will be higher than what’s quoted.
The reasons why shoulder replacement can fail include infection, component loosening, component wear, rotator cuff failure, and trauma. There are specific intraoperative steps and technical points and postoperative management/recommendations to minimize these possibilities.
TOTAL SHOULDER REPLACEMENT WITH DR. SHI
Preoperatively
- Patients will need to have a visit with the anesthesiologist, a visit with Dr. Shi and his team, and a CAT scan of the shoulder for surgery planning purposes. This usually can be done in one visit.
- Anesthesia: The anesthesiologist will discuss options with you. Most patients elect to have an interscalene nerve block, a local anesthesia in which the arm and shoulder are made numb. Additionally you have general anesthesia with a breathing tube. The pain relief with an interscalene nerve block may last well into the evening and this means you may need less pain medication immediately after surgery than if the nerve block was not performed. If there is some medical reason that you are not a candidate for a nerve block, then general anesthesia is utilized.
Surgery and hospital stay
- The surgery is usually 2-3 hours in length or longer in complicated/revision cases.
- You are admitted to the hospital afterwards. Patients generally stay 2 overnights and are discharged home in a shoulder immobilizer (i.e. sling).
- You will work with therapists in the hospital who will show you some range of motion exercises to do in the hospital and after discharge. Formal outpatient physical therapy is started 2 weeks after your surgery.
- Home services/rehabilitation hospital: Generally, our total shoulder replacement patients do NOT need home nursing and rehab hospital stay. These patients are mobile (due to having only upper extremity surgery), and since they mostly stay in a sling for the first two weeks, supervised therapy is not necessary. Depending on patients’ home/family situation and their overall health, home services or rehab hospital stay may be indicated; you should mention this to the doctor and his team before and during your hospital stay.
After discharge
- Office visits. You will visit with the doctor at 2-week mark, 6-week mark, 3-month, and 1-year after surgery. You likely will not need x-rays between the 2-week and the 1-year visits.
- Therapy/activity restrictions: You will be given a prescription at your first postop visit to start therapy at that time, approximately 2-3 times per week. You will be doing passive range of motion exercises with your therapists and at home. You will wear the sling for 4 weeks after surgery. After 4 weeks, you can come out of your sling and start active range of motion, i.e. hygiene and other activities of daily living. You will focus on motion in the first two months after surgery. Starting in the third month, you can start with strengthening, while not neglecting flexibility exercises. You may need 3 months of formal therapy, with less frequent visits towards the end of this period; individual patient varies in his/her needs. The doctor and your therapist will communicate regarding your progress throughout this time.
- Sports participation/restrictions: You are discouraged from contact sports after surgery, but you can likely resume sports such as golf and tennis after your 3-month visit. A 25-pound weight limit is recommended for lifting objects to the shoulder level and above. This is a life-long recommendation so as not create extra wear and decrease the lifespan of the prosthesis.
- Recliner: For first two weeks, many patients find it more comfortable to sleep in a recliner because the shoulder immobilizer can be hard to manage when lying flat in bed.
- Anti-inflammatory medications: Because non-steroidal anti-inflammatories can impair bone healing, we ask you to avoid medications such as ibuprofen, motrin, aleve, Naprosyn, etc, for two months after surgery.
- Antibiotics: We do recommend taking antibiotics before dental procedures (even routine cleanings) and colonoscopy for shoulder replacement patients. The official recommendations have shifted back and forth in the last decade, but our guideline is that patients need life-long infection prophylaxis. The downside of taking the medication is minimal, and downside of treating an infected shoulder prosthesis is significant. Our office can call in the medication, usually in with multiple refill. Often the dentists are willing to prescribe the antibiotics as well if s/he knows that this is our official recommendation.
- Medication is 2 gram dose of amoxicillin by mouth 1 hour prior to procedure. 600mg clindamycin is used in patients who are allergic to penicillin.